Blip-Zip Executive Summary
Health systems are intricate. This article explores System of Systems (SoS) thinking and Social Determinants of Health (SDOH) as powerful tools for improving collaboration, addressing root causes, and ultimately transforming health outcomes.
Blip-Zip Takeaways
- Unleash System of Systems (SoS) Thinking: Break down silos & foster collaboration across health & human services for a more efficient system.
- Tackle Root Causes: Address Social Determinants of Health (SDOH) like poverty & housing to improve population health outcomes.
- Unlock System Potential: Leverage SoS & SDOH to create a more responsive & adaptable health ecosystem for all.
Key Words and Themes (#Hashtags)
#systemofsystems #socialdeterminantsofhealth #HHS #SoS #SDOH #PopulationHealth #HealthcareLeadership #Collaboration #CommunityHealth #PublicHealth #StrategicLeadership #SystemsThinking
Table of Contents
Demystifying System of Systems (SoS): Interdependence in Action
The health and human services (HHS) sector faces interconnectivity issues. Chronic diseases are on the rise, populations are aging, and healthcare costs continue to climb. Addressing these challenges requires a paradigm shift from siloed, fragmented thinking to a more holistic and collaborative approach. A common challenge in systems thinking is understanding the whole “system” or big picture, followed by being overwhelmed by the magnitude of the system.
The key to systems thinking is mutual interaction, which implies something occurs between the parts to maintain the existence or performance of the system. The parts are, therefore, interdependent and interconnected. The loss or breakdown of any one part will affect the function of the whole or system of systems (SoS).1
A system of systems (SoS) is the collection of multiple independent systems and subsystems in a more extensive, complex system. Systems exhibit behaviors affecting the behavior of the whole system. These behaviors are interdependent while connected to other subsystems and cannot be separated. An Intensive Care Unit (ICU) is an organized system for care for critically ill patients. The ICU has feedback loops, stocks, flows, and delays, such as an ICU Nurse’s interactions with the medical, surgical unit, materials management, or discharge personnel who represent functions or subsystems. These interacting, interrelated, and interdependent components eventually form a unified whole or system of systems (SoS).
This description is where the concept of Systems of Systems (SoS) and a deep understanding of the Social Determinants of Health (SDOH) become critical tools for strategic health leadership (SHELDR) developmeny and application of the 17 competencies. A “system of systems” within the health and human services sectors can be defined as a virtual system comprised of a collection of separate, independent component systems that work together to achieve a common goal. Imagine a bustling city.
The transportation system (roads, buses, trains) relies on a functioning energy grid (power plants, transmission lines) to power traffic lights and keep vehicles operational. These component systems are interconnected and work together to perform functions that cannot be achieved by the individual systems alone.
Systems of Systems (SoS) In the Health and Human Services (HHS) Sectors
Similarly, the public health department (a system) depends on data from healthcare organizations (another system) to track infectious disease outbreaks. The “system of systems” framework provides a new way of understanding the interoperability of health and human services spanning multiple organizations in the context of complex inter-agency relationships. Each system retains its autonomy, but their coordinated interaction creates a more robust and efficient whole. Here are some critical characteristics of SoS in the HHS sector:
- Interdependence: Different systems rely on each other for information, resources, and services. For example, a public health department relies on healthcare organizations to report infectious disease cases, while healthcare organizations depend on public health data to implement targeted interventions.
- Decentralization: Individual systems have a degree of autonomy in their operations. Healthcare organizations manage their budgets and staff but collaborate with other systems to ensure continuity of care for patients transitioning between settings.
- Emergent Properties: The combined interaction of independent systems creates a new, higher-order capability. A network of well-coordinated community resources provides a more comprehensive support system than any individual service alone.
- Goal Alignment: All systems within the SoS share a common goal, such as improving population health outcomes or reducing health disparities.
Several health organizations engage in community partnerships and have system-wide information systems and teams of clinicians and health system integrators to provide care efficiently, reliably, and safely. Some have characterized these organizations as fully “integrated” delivery systems that own the hospitals, employ physicians, use a single information system, and play the role of health insurance plan. Examples include the Veterans Health Administration, Kaiser Permanente, Intermountain Healthcare, Cleveland Clinics, and Geisinger Health System.
A closer look at these systems reveals they are more open, thinking, and learning health systems. Through thinking and learning, systems intentionally improve and respond to opportunities in the environment as part of the more extensive system of systems. Local partnerships should be viewed as a part of a more extensive system of variables and interventions that interact to influence population health.
Learn More
Significance of SoS in HHS: Beyond Traditional Models
As part of an integrated delivery network, Social Currents’ National Imperative Report cites the vital economic, education, and social impact of human services community-based organizations (CBOs) as part of the health and human services ecosystem. Greater integration and coordination can transform CBOs, such as shifting from service provision to outcomes, improving innovation capacity, establishing generative partnerships, adopting new financial strategies, and reforming the regulatory environment.
This collaborative and SoS approach aims to achieve more significant results and improve health, well-being, and community success. Figure 1 illustrates SoS thinking and empowers strategic health leaders to constantly seek continuous improvement in the integration of HHS CBOs by:
Figure 1: HHS Ecosystem
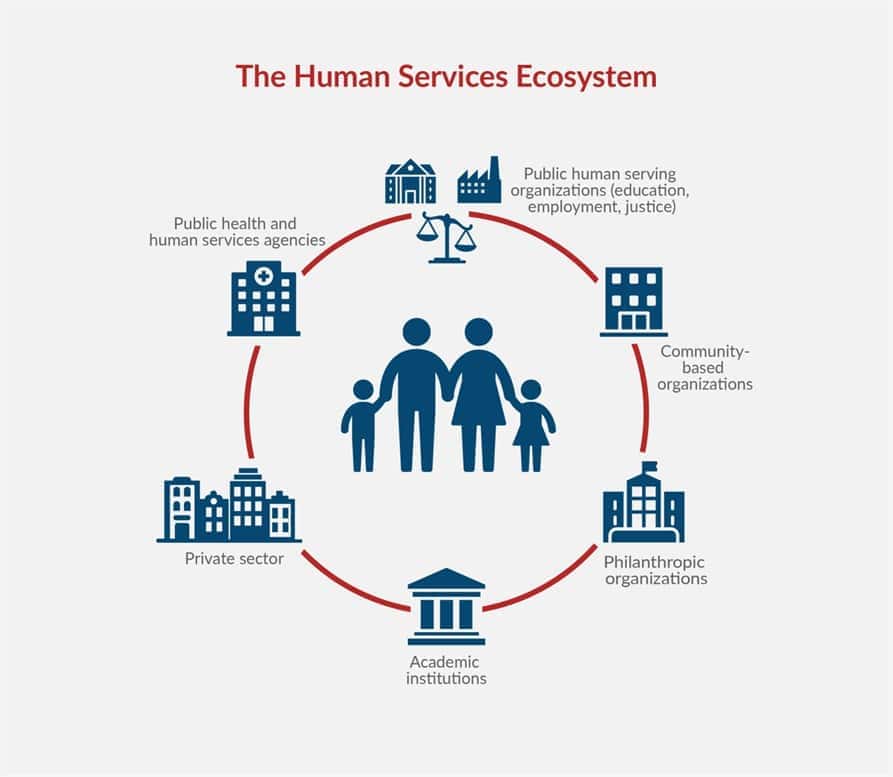
Identifying Root Causes: By understanding interdependencies within the SoS, leaders can move beyond treating symptoms. Frequent healthcare organization readmissions for congestive heart failure might link to inadequate patient education or lack of social support at home – issues that fall outside the traditional purview of a healthcare organization system alone.
- Designing Collaborative Interventions: SoS promotes collaboration across sectors. A healthcare organization can partner with social services to provide housing assistance to patients with heart failure, reducing readmission rates.
- Optimizing Resource Allocation: Resources can be distributed more effectively when leaders understand how various systems interact within the HHS SoS. This approach can help identify service provision gaps and allocate resources to address them.
- Promoting Resilience: SoS fosters a more resilient ecosystem. When one system experiences disruption, others can compensate, minimizing the overall impact. For example, during a pandemic, telehealth services provided by a clinic can help pay for reduced in-person visits at healthcare organizations.
Despite many HHS CBOs’ financial stress, many stakeholders are optimistic and make a strong case for changes to build stronger, resilient, healthier individuals and families with more significant economic and social returns. HHS CBOs, all levels of government, and the philanthropic sector must work together to solve these complex problems. To achieve these returns, our nation must embrace and invest in HHS CBOs, mitigate the barriers, and advance initiatives to help the SoS or HHS ecosystem achieve achievable results.
Systems and Subsystems in the Health and Human Services Ecosystem
The health and human services (HHS) sector is an intricate tapestry woven from diverse subsystems. Understanding these subsystems through a SoS and subsystems lens is crucial for strategic leadership and effective service delivery. Table 1 provides a breakdown of subsystems.
Table 1: Subsystem, Examples and Characteristics
| Subsystem | Examples and Characteristics |
| Closed Systems: A Flawed Ideal: A closed system operates in isolation, with minimal to no exchange of information or resources with its environment. It is a theoretical ideal that rarely exists in reality, especially within HHS. | While not entirely representative, a hypothetical healthcare organization with zero communication with the outside world could be considered a closed system. There would be no exchange of medical advancements, patient referral networks wouldn’t exist, and essential supplies might become unavailable. The lack of interaction with the environment impedes a closed system’s ability to adapt and evolve. This could hinder patient care, innovation, and responsiveness to community needs. Closed systems within HHS would create silos, inhibiting collaboration and restricting the overall effectiveness of the ecosystem. |
| Natural Systems: The Body’s Inner Workings: Natural systems are self-regulating, complex networks of interacting components within a living organism. In HHS, the human body itself is a prime example of a natural system. | The human body comprises intricate systems, such as the immune, cardiovascular, and nervous systems. These systems interact and communicate constantly to maintain homeostasis (internal balance). The body interacts with the environment in numerous ways. It takes in oxygen and nutrients, eliminates waste, and is influenced by stress, diet, and exercise. Understanding natural systems within the body allows healthcare professionals to tailor interventions and provide holistic care. |
| Designed Systems: Tools for Specific Needs: Designed systems are human-made creations with specific functions. Though not inherently complex, they can become interdependent within a more extensive system. | While a treadmill is designed, it becomes part of a broader system when integrated into a physical therapy program within a healthcare organization. Designed systems become interdependent when they are integrated into a more extensive system. The treadmill, for instance, relies on a functioning electrical grid and maintenance staff for proper operation. Designed systems, like medical equipment or electronic health records, can enhance efficiency and service delivery when integrated effectively into the HHS ecosystem. |
| Open Systems: The Heart of HHS: Open systems interact with their environment, exchanging resources (personnel, supplies, information) to survive and thrive. These characteristics are crucial for effective functioning in the HHS sector. | Healthcare organizations are prime examples of open systems. They receive patients from the community (environment), utilize resources (drugs, technology) from suppliers, and share medical knowledge with other institutions, fostering collaboration and improved care. Continuous interaction with the environment is a defining characteristic of open systems. Public health departments, for instance, interact with the county and community to address social determinants of health (SDOH). Addressing SDOH, like access to healthy food or safe housing, can significantly impact health outcomes. Open systems are the cornerstone of a thriving HHS ecosystem. Their ability to adapt, share resources, and learn from each other contributes to improved population health outcomes. |
| Continuous Learning Systems: Embracing Change: Continuous learning systems are dynamic, open systems that constantly acquire new knowledge, adapt, and innovate. Continuous learning systems have a second unique characteristic: the creative ability to use what is known, go beyond the level of expectations, and create disruptive innovations or breakthrough processes.2 This is a crucial characteristic for any subsystem within the HHS sector. | Continuous learning systems encourage experimentation, share best practices, and embrace feedback loops. They prioritize lifelong learning so that professionals stay updated on the latest advancements. Innovation is a hallmark of continuous learning systems. Artificial intelligence (AI) can play a significant role by analyzing large datasets to identify trends, predict outcomes, and personalize interventions. Continuous learning systems drive innovation and improvement within the HHS ecosystem. New technologies, treatment protocols, and service delivery models can emerge through constant learning and adaptation. |
Three key characteristics are crucial for effective functioning regardless of the subsystem type. First, Adaptability, or the ability to adjust to changing environments, is critical. A healthcare organization that can adapt to new infectious diseases or patient needs will be more successful. Second, Systems require feedback mechanisms to monitor progress and make adjustments. A healthcare organization analyzing patient satisfaction surveys uses feedback loops to identify areas for improvement. Lastly, all subsystems within HHS should be aligned towards a common goal – improving population health and well-being.
Understanding the different types of subsystems within HHS and their interactions is crucial for promoting a holistic approach to health and well-being. By fostering open systems that exchange information, adapt to change, and embrace continuous learning, the HHS ecosystem can create a healthier future for all. We will see more of these systems as robotics and artificial intelligence (AI) continue infusing our lives. AI will soon, and already has, in many ways, augment human thinking, not simply for efficiency but also enhanced creativity.
Unpacking the HHS Ecosystem: A Look at Subsystems
Understanding these subsystems and their interactions is crucial for effective leadership and service delivery. Subsystems are distinct components within a more extensive system that contribute to its overall function. Within the HHS sector, subsystems represent specific focus areas, such as healthcare delivery or social services. These subsystems operate independently but maintain critical connections to ensure a holistic approach to well-being. Table 2 provides a breakdown of some critical subsystems within HHS:
Table 2 HHS Subsystems
| HHS Subsystems | Roles and Functions |
| Public Health: Focuses on preventing disease outbreaks, promoting health education, and ensuring community preparedness for health threats. | Public health monitors and protects population health, investigates disease outbreaks, and promotes healthy behaviors. A public health department conducts community outreach programs on vaccine importance and monitors local disease trends. |
| Healthcare Delivery: Encompasses healthcare organizations, clinics, and other providers who diagnose and treat illnesses. | Diagnoses and treats medical conditions, provides preventative care, and manages chronic diseases. A healthcare organization system includes emergency care, surgery, and inpatient services for various medical conditions. |
| Behavioral Health: Addresses mental health and substance abuse issues through therapy, medication, and addiction treatment programs. | Identifies and treats mental health and substance abuse issues, promoting emotional well-being and recovery. A community mental health center offers individual and group therapy sessions for depression and anxiety. |
| Social Services: This department provides essential support services such as food assistance, housing assistance, and job training to low-income individuals and families. | Provides a safety net for vulnerable populations, offering essential services to meet basic needs and promote social integration. A social service agency helps individuals experiencing homelessness secure temporary shelter and access resources for permanent housing options. |
| Long-term care offers assistance with daily living activities for older adults or people with disabilities who require support at home or in residential facilities. | Supports individuals who require assistance with daily living activities, ensuring their well-being and independence. A home health care agency provides nurses and aides to assist patients with bathing, dressing, and medication management in their own homes. |
| Public Health Insurance: Government-sponsored health insurance programs like Medicare and Medicaid provide health coverage for low-income individuals, seniors, and people with disabilities. | Provides financial coverage for healthcare services, enabling individuals to access necessary medical care. Medicare covers healthcare organization stays, physician visits, and other medical services for people aged 65 and over. |
Subsystems within HHS are not isolated entities. They interact and collaborate in various ways. First, Public Health shares information with Healthcare Delivery about potential outbreaks, requiring coordinated response efforts. Second, Behavioral Health may partner with Social Services to address the social determinants of mental health issues, such as poverty or housing instability. Third, Long-Term Care facilities often collaborate with Healthcare Delivery to ensure continuous care for chronic conditions. Finally, Public Health Insurance programs financially support Healthcare Delivery services, providing financial accessibility.
Effective communication, data sharing, and collaboration across these subsystems are crucial for achieving optimal health outcomes. The HHS ecosystem can deliver comprehensive services, address individual and community needs, and promote overall well-being by working together.
The Upstream Strategic Health Leadership Imperative

For example, a problem like preadmission penalties or harm prevention can be the “system .”However, external contexts or upstream factors include payment policies, families as caregivers, and structures, like how patients move through the systems to alternative settings. Prevention of harm or readmissions goes beyond healthcare organizations. These problems and opportunities should challenge leaders to systematically rethink their value proposition, such as the relentless pursuit of zero harm before admission, during care, discharge to a home or health setting, and patient/family engagement.
SDOH often operates upstream, influencing health long before people experience symptoms. For example, a person living in poverty may struggle to afford nutritious food and quality housing, increasing their risk of chronic diseases like diabetes and heart disease. Their risk of premature death rises too. Addressing SDOH is crucial for strategic health leadership because of its significant impact on health outcomes:
- Chronic Disease Risk: Chronic stress associated with poverty or unsafe neighborhoods can contribute to a higher risk of chronic diseases like heart disease, diabetes, and mental health issues.
- Health Disparities: People with lower socioeconomic status, less education, or living in disadvantaged communities often experience poorer health outcomes. This situation creates a cycle where lack of resources leads to poorer health, further limiting opportunities to escape poverty.
- Unsustainable Healthcare Costs: Addressing SDOH can save money in the long run. Preventing chronic conditions and promoting healthy living can reduce healthcare costs. Imagine if fewer people needed frequent healthcare organization readmissions due to complications from preventable diseases.
Top causes of death have a specific risk factor that can be reduced with changes in lifestyle and by addressing chronic health issues. Table 3 illustrates how communities can systemically reduce premature death.
Table 3 Disease and Community Program
| Disease | Community Program |
| Heart disease: tobacco use, high blood pressure, high cholesterol, type 2 diabetes, poor diet, overweight and lack of physical activity | Kick It California: We’re a free program that helps Californians kick smoking, vaping, and smokeless tobacco with the help of proven, science-based strategies. |
| Cancer: tobacco use, poor diet, excessive consumption of alcohol, lack of physical activity, overweight, sun exposure, and exposure to certain chemicals and other substances | The SunSmart Schools program is a national initiative with local implementation. It aims to educate children and staff about sun safety practices and reduce the risk of skin cancer. |
| Chronic respiratory disease: tobacco smoke, exposure to second-hand smoke, indoor air pollutants, outdoor air pollutants, and allergens | Breathe California is a statewide organization with local chapters that work to improve air quality and reduce exposure to air pollutants that contribute to respiratory problems. |
| Stroke: high blood pressure, high cholesterol, heart disease, diabetes, overweight, tobacco and alcohol use, and lack of physical activity | High Blood Pressure and High Cholesterol:The American Heart Association offers blood pressure and cholesterol screening programs across the country. |
| Unintentional injury: lack of seatbelt use, lack of motorcycle helmet use, misuse of consumer products, alcohol and drug abuse, and unsafe home and community environments | Safe Kids Worldwide is a national organization with local chapters working to prevent childhood injuries, including misuse of consumer products. |
Other examples of addressing SDOH for Better Health may include Kaiser Permanente’s Community Health Hub, where you can see a doctor, get help with housing, and access nutrition counseling – all under one roof! Ohio’s School-Based Health Centers integrate health services directly into schools to remove student care barriers. Services can include physicals, mental health support, and even referrals for social services. JAMA states that these centers contribute to a healthier learning environment and health outcomes and that they should be expanded.
Find a Health Center helps you search for HRSA-funded health centers. I
How Strategic Health Leaders Will Transform The HHS Ecosystem
Understanding the components and overall goals of the systems of systems framework can help strategic health leaders transform the HHS ecosystem in several ways:
Table 4: SoS Framework Components
| Components | Examples |
| Interoperability: This provides a new way of understanding the interoperability of health and human services across multiple organizations. This understanding can help leaders develop strategies to improve the seamless exchange of information and services between different agencies and systems. | Standardizing electronic health records (EHR) across hospitals, clinics, and public health departments allows seamless sharing of patient information, improving care coordination and reducing duplication of services. Integrating mental health data from community clinics with hospital discharge data can provide a more holistic view of a patient’s health and continuity of care. |
| Complexity: Allows leaders to comprehend the complex inter-agency relationships within the health system. This understanding can aid in developing strategies to enhance collaboration, coordination, and communication among diverse agencies, leading to more efficient and effective delivery of health and human services. | A network of hospitals, clinics, social service agencies, and public health departments working together to address a community’s opioid addiction crisis. Each agency brings expertise and resources, requiring strong communication and coordination to achieve a common goal. CMS’s policy addressing social determinants of health (SDOH), like poverty or food insecurity, involves collaboration between HHS agencies, housing authorities, and community organizations. |
| Synergy: This term highlights emergent synergistic behavior, where the functionality of the system of systems is greater than the sum of its individual components. Strategic health leaders can leverage this understanding to identify opportunities for creating synergies and optimizing the overall performance of the health system. | Integrating telehealth services offered by a hospital with transportation assistance provided by a social service agency allows patients in remote areas to access essential healthcare services. This opportunity creates a more comprehensive system than either service could offer alone. Combining disease surveillance data from public health with insurance claims data can identify emerging public health threats and inform targeted interventions. |
| Adaptive: Acknowledges the evolutionary development of systems of systems, emphasizing the need for adaptive and flexible approaches to system transformation. Strategic leaders can use this understanding to implement agile and responsive strategies that accommodate the evolving needs and challenges of the health system. | A public health department is developing a flexible vaccination strategy to respond to new virus variants. This might involve using mobile vaccination clinics and offering extended clinic hours to adapt to changing community needs. A hospital is implementing a new electronic health record system (EHR) that allows for easy integration of future upgrades and new functionalities to remain adaptable to evolving technologies. |
| Integration: Provides insights into the integration environment of health and human services systems, enabling leaders to assess and improve the policies, technologies, and processes that facilitate seamless integration and collaboration among different agencies and systems. | Establishing a common data platform across HHS agencies allows for efficient information exchange and facilitates collaboration between different programs. Standardized referral processes between hospitals, mental health clinics, and addiction treatment centers ensure that individuals receive a seamless continuum of care. |
Understanding the SoS framework equips strategic health leaders with a comprehensive perspective on the health system’s complexities and dynamics, empowering them to develop and implement transformative strategies that enhance interoperability, collaboration, and overall system performance.
Summary and Conclusion
We explored Systems of Systems (SoS) and Social Determinants of Health (SDOH) as powerful tools for strategic health leaders. It revealed how SoS thinking fosters collaboration across HHS sectors, while SDOH tackles root causes of health disparities.
By embracing SoS thinking and addressing SDOH, health leaders can create a more collaborative and effective healthcare system. This means treating illnesses and addressing the “place” where health happens—our communities. So, the next time you visit a doctor or community center, remember: it’s all part of a bigger system working to keep you well! By embracing both, leaders can create a more responsive and equitable health ecosystem.
Ready to transform your health leadership? Explore the resources below to dig deeper into SoS, SDOH, and practical application in your leadership journey!
Deep Dive Discussion Questions
- Reflect on Your Leadership Style: How can you leverage SoS principles to improve collaboration within your organization and across the broader HHS ecosystem?
- Identifying Root Causes: Consider a pressing health challenge in your community. What social determinants of health (SDOH) might be contributing factors?
- Actionable Strategies: Develop a hypothetical plan to address an SDOH in your community. Who would be key partners? What resources would be needed?
- The Power of Data: How can data sharing and analysis across HHS systems be optimized to improve population health outcomes?
- The Evolving Landscape: Healthcare is constantly evolving. How can strategic health leaders maintain an adaptive approach within an SoS framework?
Professional Development and Learning Activities
- Self-Assessment: Conduct a self-assessment of your leadership style. Identify areas where SoS principles can be incorporated for improved collaboration.
- Community Collaboration: Reach out to other HHS organizations in your community. Identify potential areas for collaboration to address local health challenges.
- Data Exploration: Explore publicly available datasets related to SDOH in your community. Identify potential correlations with health outcomes.
- Leadership Development Courses: Consider enrolling in leadership development courses that focus on collaboration and complex systems thinking.
- Mentorship: Seek mentorship from experienced leaders who champion SoS and SDOH principles.
References and Resources
- The National Imperative Report (https://www.social-current.org/news/)
- JAMA on School-Based Health Centers (https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2809634)
- Find a Health Center (https://findahealthcenter.hrsa.gov/)
- Centers for Disease Control and Prevention’s Social Determinants of Health https://www.cdc.gov/publichealthgateway/sdoh/index.html
- The Robert Wood Johnson Foundation’s Commission to Build a Healthier America https://www.rwjf.org/en/grants/grantee-stories/programs/rwjf-commission-to-build-a-healthier-america.html
- The National Academy of Medicine’s Action Collaborative on Social Determinants of Health https://nam.edu/action-collaborative-on-clinician-well-being-and-resilience-network-organizations/
- Centers for Disease Control and Prevention’s Social Determinants of Health (https://www.cdc.gov/about/sdoh/index.html) This CDC webpage provides a comprehensive overview of SDOH and their impact on health outcomes.
- The Robert Wood Johnson Foundation’s SDOH County Health Rankings (https://www.rwjf.org/en/grants/grantee-stories/programs/county-health-ranking-roadmap.html) This website allows users to compare health outcomes and social determinants of health across different counties in the United States.
- Kaiser Permanente Community Health Hub (https://about.kaiserpermanente.org/commitments-and-impact/healthy-communities/news/social-health-help-is-just-a-click-or-call-away) This Kaiser Permanente initiative provides a real-world example of integrating healthcare with social services under one roof.
- The Center on Budget and Policy Priorities’ Medicaid and the Social Determinants of Health (https://www.cbpp.org/research/topics/medicaid-and-chip) This CBPP report explores the role of Medicaid in addressing SDOH.
Citations
1. Bellinger G. Systems Thinking: an Operational Perspective of the Universe. In. Outsights.1998.
2. Bruner J. Going Beyond the Information Given. New York: Norton; 1974.