Is your leadership style contributing to the urgent healthcare crisis in your community?
Blip-Zip Executive Summary
Despite medical advancements, significant health disparities persist. This article discusses the role of Strategic and Upstream Health Leadership (SHELDR) in addressing these disparities. SHELDR, by integrating Social Determinants of Health (SDOH) such as housing and education, fosters a culture of health and well-being for all. It’s time to explore how SHELDR can transform your community’s health system.
Blip-Zip Takeaways
- Strategic Health Leadership (SHELDR): A crucial strategic-thinking approach that integrates social determinants of health to improve community health outcomes.
- Social Determinants of Health (SDOH): Understanding how housing and education influence health is crucial for a comprehensive health strategy.
- Building a Culture of Health: SHELDR fosters collaboration within communities to create a holistic approach to well-being.
Key Words/Hashtags (#)
#SHELDR #StrategicHealthLeadership #upstreamleadership #SocialDeterminantsofHealth #SDOH #CommunityHealth #HealthEquity
Table of Contents
Introduction To Building Integrated Community Health Systems
Why do communities still face disparities in health outcomes despite advancements in healthcare? This question lies at the heart of strategic and upstream health leadership, a transformative approach that addresses, manages, coordinates, and integrates social care services and other social determinants of health (SDOH) between your organization and community-wide agencies.
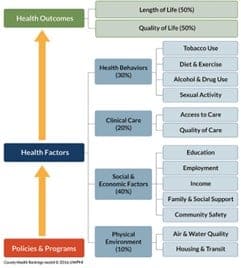
For example, the COVID-19 pandemic exposed what we already knew but have ignored for decades: the divide between the healthcare or “sick care” system and “fix me now” society rather than an integrated community health system: lack of value-based Care, investment in preventive health and a “culture of health” or personal responsibility approach is what is killing the healthcare systems. The SDOH is estimated to influence around 80% of health outcomes versus 20% attributed to clinical Care. Unsurprisingly, as depicted in the County Health Rankings model below, the communities most challenged by social risk factors are most vulnerable to COVID-19.
The Imperative for Integration
Integrating SDOH into healthcare strategies is not just beneficial; it’s urgent. With the rise of chronic diseases and healthcare costs, the need for a holistic approach to health is pressing and cannot be ignored.
More specifically, the key to success is improving access to and coordinating referral services between hospitals and social care organizations. According to the American Association of Physician Leadership (AAPL), most physicians know how critical social determinants can be and wish they could do something about them. Among patients’ most glaring needs are fitness programs, nutritious food, and transportation assistance. Urban doctors emphasize employment, adult education, and housing assistance.
But how can this be achieved, and why is it crucial for the future of a health culture? First, leaders need to shift their mindset beyond the walls of their organization to their communities and regions. Second, applying strategic health leadership principles is not just important, it’s your responsibility. Finally, the strength of will implement, sustain, and learn from the effort if it is absolutely necessary.
Read more
The Imperative: Strategic Health and Upstream Leadership
Be honest with yourself. What if your board of directors tasked you with improving the coordination of referral services between your organization and community-wide agencies?
Do you have what it takes to be a health system executive or strategic health and upstream leader?
Many leaders reach their senior-level positions based on their success as operational-level managers. They bring great skills to the table, but they are not enough. Sadly, for many of these leaders, the development of these skills may be too late.
The infographic titled “10 Principles of Strategic Leadership” outlines essential strategies for leaders aiming to foster innovation and resilience within organizations. These principles emphasize distributed responsibility, transparency, idea incubation, embracing failure as a learning opportunity, networking with strategists, experiential learning, transformative hiring practices, authenticity, reflective practice, and recognizing leadership as a continuous journey. You can also review my article on how to get beyond a transactional or firefighter leadership styles.
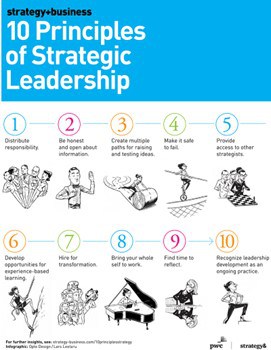
Applied to strategic health leadership (SHELDR), these principles guide the integration of social determinants of health (SDOH) into strategic planning, ensuring that healthcare systems and social care organizations work collaboratively to improve community health outcomes.
Strategic and upstream health leadership transcends traditional healthcare management. It represents a proactive philosophy, emphasizing collaboration, long-term planning, and innovative solutions to address the root causes of health issues within a population. This leadership style prioritizes upstream thinking, which focuses on preventing health crises by addressing the social determinants of health (SDOH).
SDOH encompasses various social and economic factors – poverty, safe housing, education access, and others – significantly influencing health outcomes. Strategic and upstream leaders view these factors as modifiable targets for intervention. Here are a few examples of how this leadership approach translates to action:
- Multi-Sectoral Collaboration: Leaders forge partnerships between healthcare providers, social services, government agencies, and community organizations. This fosters a holistic approach to addressing the complex interplay of factors affecting community health.
- Data-Driven Decision-Making: Leaders utilize data analytics to understand community needs and measure the effectiveness of interventions. This enables them to optimize resource allocation and prioritize programs with the most significant impact.
- Innovation and Long-Term Vision: Strategic leaders seek and implement innovative solutions like preventive programs for substance abuse, initiatives promoting healthy food access, and affordable housing projects. These investments offer long-lasting positive effects on community health outcomes.
By addressing the underlying factors that contribute to poor health, strategic and upstream health leadership fosters resilient communities. This approach empowers leaders to cultivate a healthier future for their populations through a preventive and collaborative lens.
Learning From and Adapting From Success
Pursuing a fully integrated community health system necessitates ongoing innovation and adaptation. Fortunately, reports on how to build successful programs provide valuable insights for strategic and upstream health leaders. Here is a set of initiatives demonstrating how a collaborative approach, data-driven decision-making, and a focus on social determinants of health (SDOH) can significantly improve community health outcomes.
- Community Resource Referral Platforms have streamlined the process of connecting patients with social services, demonstrating improved efficiency and patient outcomes.
- The Department of Health and Human Services Community Care Hub approach has shown that a coordinated network of community-based organizations (CBOs) can effectively improve health outcomes.
- Partnerships highlighted by the Center for Health Care Strategies have developed case studies that examine successful collaborations.
- According to the Institute for Accountable Care, the Hub and Spoke Model used by CBO networks simplifies contracting and referral processes, integrating with electronic health records for seamless service delivery. A growing evidence base demonstrates that addressing patients’ social needs can improve health outcomes and facilitate appropriate utilization of health care services.
- The Agency for Healthcare Research and Quality white paper on Coordinating Care in the Medical Neighborhood: Critical Components and Available Mechanisms highlights how referral processes have been established, with hospitals and social services working together on community programs, enhancing overall community health.
By gleaning knowledge from these successful models and adapting them to local contexts, healthcare leaders can propel integrated systems forward, ultimately fostering a culture of health and well-being for all. The journey of integrated health systems and strategic health leadership development is ongoing.
A Call to Action
Integrating strategic and upstream health principles into community-wide planning is not just a theoretical ideal; it’s a practical necessity. The principles of strategic leadership provide a blueprint for this integration. By distributing responsibility and creating safe spaces for idea generation, health leaders can foster a culture where every stakeholder has a role in shaping health outcomes. Continuous development and application of upstream health principles are vital for adapting to the ever-changing landscape of creating a culture of health. Leaders must remain agile, learning from successes and failures, to drive the mission of integrated health systems forward.
Read more
As we reflect on the success stories and the principles that guided them, let’s ask ourselves:
- How can we further distribute leadership to empower more stakeholders?
- What new pathways can we create for innovation in health integration?
- How can we make our health systems more reflective and adaptive?
References and Resources
- Community Resource Referral Platforms: A Guide for Health Care
- Community Care Hubs: Making Social Care Happen
- Supporting Health Care and Community-Based Organization Partnerships
- Community-Based Organizations Are Important Partners for Health Care
- Establishing a Solid Social Service Referral Process
Let’s continue building on these foundations, striving for a future where everyone can have optimal health and well-being.




