Blip-Zip Executive Summary
Tired of a failing healthcare system? The Gimme SHELDR! Strategic Health Leaders (#SHELDR) are the answer! Develop critical thinking & collaboration skills to fix the “wicked” problems plaguing healthcare. Learn more!
Blip-Zip Takeaways
- Join the Journey to Master the Habits of Effective Strategic Health Leaders
- Think Critically & Collaborate to Solve Healthcare’s Toughest Challenges
- Become a Transformational Leader & Fix the Broken Healthcare System
Top 5 URL Focus Keywords/Themes (with Hashtags)
Strategic Health Leadership (#SHELDR), Healthcare Leadership Development (#LeadershipDevelopment), Transforming the Healthcare System (#HealthcareTransformation), Building a Healthier Nation (#PublicHealth), Social Determinants of Health (#SDOH)
Table of Contents
P1: Purpose of GIMME SHELDR (Strategic Health Leadership)!
In the words of Mick Jagger, “GIMME SHELDR!” I will reiterate what I stated early on concerning establishing the Strategic Health Leadership (SHELDR) Institute and my passion to create and develop strategic-minded leaders earlier, more often, and in more significant numbers. The passion was borne out of the following presentations and articles. You may download the following using this LINK:
- Presentations: 2017 and 2018 American College of Healthcare Executives (ACHE) Congress presentations on GIMME SHELDR!
- Presentation: Presentation Extract On Development Of A Leadership Ethos And Leader Development Ideas
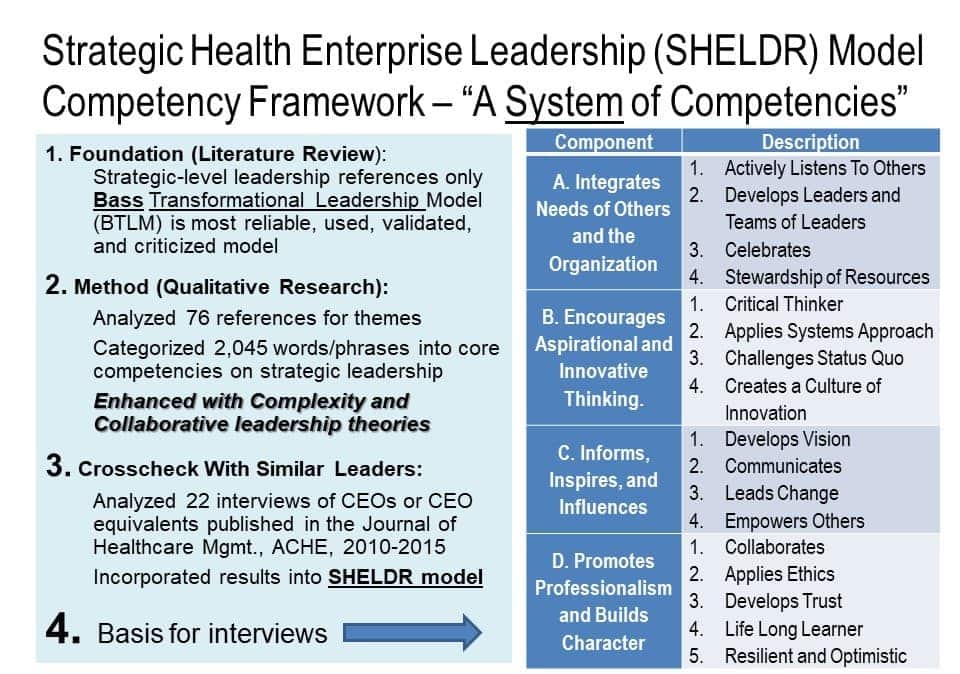
- Article: Strategic Leadership: A Study Of Strategic Health Leadership (SHELDR) Practices Among Former U.S. Military Surgeons General (14)
Through my consulting, coaching, research, and continuing studies, plus a factual review of the state of the U.S. healthcare system before and after the pandemic, I am more convinced than ever that a new brand of leadership–Strategic Health Leadership (SHELDR) and a systemic approach is required to fix the “wicked” nature —a chronic, complex, unsafe, unreliable, costly, wasteful, unsustainable, and frustrating—of the U.S. health system.
Most things stayed the same in 2023 or post-pandemic. In fact, in 2011, according to the Commonwealth Fund’s Report, 37 indicators of performance, the U.S. achieved an overall score of 64 out of a possible 100 when comparing actual performance to benchmarks.
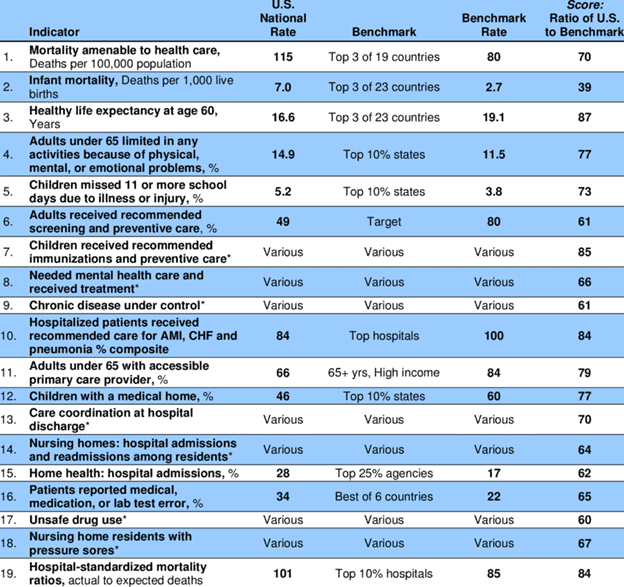
Source: National Scorecard on U.S. Health System Performance
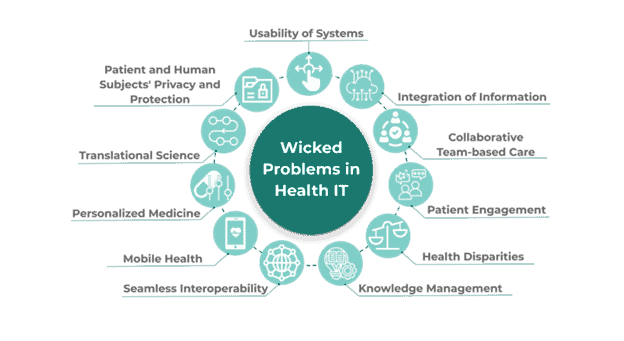
We can do better; however, we must acknowledge that leadership and leadership development are the root causes of a complex, faltering system. Complexity has a profound effect on health outcomes. Multiple dimensions, including co-occurring or multifaceted medical conditions, age, frailty, socio-economic realities, culture, environment, behavior, and systems factors characterize complexity. This purposive, thematic review describes aspects of health care complexity… Or wickedness.
To put it another way, a “wicked problem” is a social, cultural, or institutional issue that is difficult to resolve despite efforts to do so. A variety of factors may contribute to the occurrence of these issues. In healthcare, wicked problems can arise for various reasons, including but not limited to divergent objectives of stakeholders, fluctuating standards and requirements, and intricate interdependencies.
It is time to transform the ailing U.S. health system into the most reliable and innovative one with the world’s healthiest nation.
P2: Problem
Although thousands of publications exist on strategic, transformational, collaborative, and complex leadership, only some focus on the environment of healthcare and its leaders.
Comprehensive studies of strategic-level health leadership and cohorts of senior health leaders have yet to be created. The degree to which anything is “wicked” is contingent upon factors such as the difficulty in monitoring and evaluating public health results, the disjointed governance of relevant services, and the conflicting interests and expectations of community members and stakeholders. Yet, we see very few studies on Strategic Health Leadership (SHELDR) competencies and the need to embrace a new breed of leadership.

Further, a bottleneck is health leader development practices. Creating strategic-minded leaders earlier and in more numbers is required. Numerous studies cite health leader development gaps associated with individual performance at higher levels of progression and complexity. Despite the devastation of Covid and exposure of the health system for what it truly is, we must be committed to a new era of leadership, especially in the most challenging times. As COVID-19-required command-and-control structures give way, the groundwork is there for us as health leaders to embrace a new era of leadership to develop an era of a diverse and empowered workforce and a culture that aligns with the values we want to instill. Leading in crisis is an opportunity to build the best culture for our providers, researchers, educators, and patients.
In my earlier article on the Tenfold Healthcare Crises, I argued that the root cause is the continued application of industrial-era leadership or command-and-control theories in an era of volatility, uncertainty, complexity, and ambiguity (VUCA) and a fixation on healthcare rather than creating better health, wellness, and resilience for individuals, families, and communities. Adopting a transformative leadership approach and being open to learning can ensure that health organizations succeed in VUCA-driven health systems.
This crossroads, or should be a crossroads of leadership and leader development, has been underscored in several programs and settings. For example, a study that investigated leadership competencies for developing senior and emerging leaders in Health Research Organizations (HROs) was conducted only to conclude that the development of strategic-minded leaders is required. The National Center for Healthcare Leadership’s’ Health Leadership Competency Model’ was used as the foundation of competency research in this study.
The findings of the HRO study determined that senior health executives need financial skills and scientific achievement. Emerging leaders need technical competence, strategic thinking, and collaboration skills. About half of the respondents reported having no leadership development program. Almost all reported that their organization encourages mentoring, but few reported an active formalized mentoring program. The study stated,
“Successful leaders will need to become more strategic, entrepreneurial, and resourceful in developing research alliances, executing research operations, and continually improving performance at all levels of the HRO.”
This new breed of leadership, Strategic Health Leadership (SHELDR), must learn how to counter VUCA and transform the health system. To counter a VUCA world, leaders should focus on vision, understanding, clarity, agility, and adaptability. They should focus on core values and interdependence with communities and regions, understand healthcare’s influential factors, establish aspirational long-term goals, and continuously learn to produce better health outcomes.
P3: Passion
I believe better in inspired, informed, and prepared leaders, especially those at the strategic health or complex health system or interagency levels–adept at systems, agile, adaptive thinking, and transformational or change leadership. These leaders must be able to stimulate, motivate, and influence others within and across organizational boundaries, which is critical. They are in short supply.
Through its Society for Healthcare strategy and market development function, the American Hospital Association has underscored the need for more prevalent adaptability, collaborative open communication, conflict management, continuous learning, discernment/judgment, influence, interpersonal savvy, and innovation. Ergo, there is a need for strategic health leadership (SHELDR) competency development.
A start would be to study successful health leaders—their impacts, experiences, insights, and preparation—and share them with aspiring strategic-level leaders who want to be more strategic-minded. These studies and observations should be followed by thought leadership and developmental programs.
P4: Performance
The pandemic’s public health and economic effects continue to affect many people. During the pandemic, millions have lost jobs or income and have difficulty paying bills, including basic needs. These challenges affect people’s health and well-being.
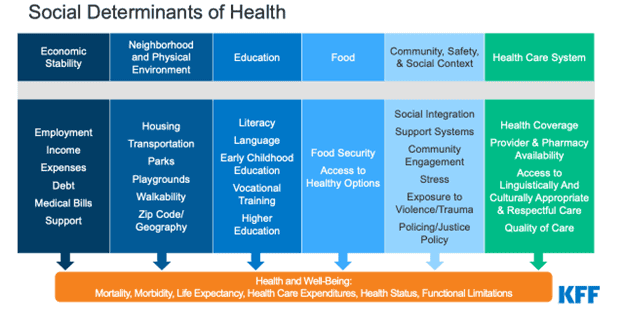
In addition to exposing the root causes of an already failing health system, the pandemic exposed its fragility as well. If anything, it exposed the fact that U.S. policymakers place too much emphasis on the Fix Me Now or healthcare system and not enough on the upstream or preventative portion of the health system to include the social determinants of health (SDOH).
While federal legislation has provided billions in funding to address the pandemic’s public health crisis and to provide economic support to low-income people struggling to make ends meet, leadership is required to produce better health outcomes in the long run.
The Strategic Health Leadership (SHELDR) Institute Websitecontains services, blogs, articles, commentaries, whitepapers, and publications—it will share why and how to apply SHELDR competencies to create better health, such as leveraging and integrating the social determinants of health (SDOH).
The goals are to develop more strategic-minded leaders and make current leaders more effective. Much of the content derived from my dissertation, research, and experience will center on the environment, trends, most prominent competencies, barriers, lessons, and successes associated with SHELDR development. As an example, my studies generated the following strategic health leadership competencies.
S1: Significance and Summary
Many would argue that health, not healthcare, is the national strategic imperative. Advancing an understanding of strategic health leadership in the context of today’s challenges will result in better-prepared leaders. Transferable insights for all healthcare sectors will be derived: strategic-minded leader development, selection of future leaders, and leader education.
Are you in? Comments?
Ready to embark on your Strategic Health Leadership journey?
Deep Dive Discussion Questions
These questions delve deeper into the concepts explored in the article, prompting you to reflect on your own leadership style and how you can apply SHELDR principles.
- Reflect on a leadership challenge you faced. How could a SHELDR approach have helped you navigate the situation?
- Consider your current strengths and weaknesses as a leader. How can you leverage your strengths and address your weaknesses to become a more strategic health leader?
- Imagine you are building a team to tackle a complex healthcare issue. What characteristics and competencies would you look for in your ideal team members?
Professional Development and Learning Activities
These activities provide practical exercises to solidify your understanding of SHELDR and develop your leadership skills.
- Conduct a self-assessment using a leadership competency framework like the National Center for Healthcare Leadership Model. Identify areas for growth and create a development plan.
- Observe a respected leader in your field. Analyze their actions and decisions through the lens of SHELDR principles.
- Participate in a leadership development program or workshop on strategic thinking, collaboration, and change management.
SHELDR Archives
- October 2025
- July 2025
- May 2025
- April 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- August 2023
References and Resources
- The Commonwealth Fund: High Performance Health System National Scorecard (https://www.commonwealthfund.org/publications/scorecards) – This resource from The Commonwealth Fund, a non-profit private foundation focused on improving healthcare quality and equity, publishes the National Scorecard on U.S. Health System Performance. This scorecard compares the performance of the US healthcare system on 43 indicators across ten key domains of performance. The scorecard allows for benchmarking the US against high-performing countries and identifies areas for improvement.
- National Center for Healthcare Leadership: Health Leadership Competency Model (https://www.nchl.org/) – The National Center for Healthcare Leadership (NCHL) has developed a comprehensive framework outlining the essential competencies for effective healthcare leadership. This model identifies eight core competencies that leaders must possess to navigate the complex healthcare landscape.




